- What is Type 1 Diabetes?
- Why a Team Approach Matters
- Diabetes Care Plan
- Managing Blood Sugar
- Using Insulin
- Exercise Tips
- Traveling with Diabetes
- Injuries and Blood Sugar Control
- Weather and Diabetes
- Preventing Long-Term Complications
- Staying Safe
- Long-Term Success
What is Type 1 Diabetes?
Type 1 diabetes is a condition where the body can’t produce insulin. This leads to high blood sugar levels.
It usually starts in childhood or young adulthood.
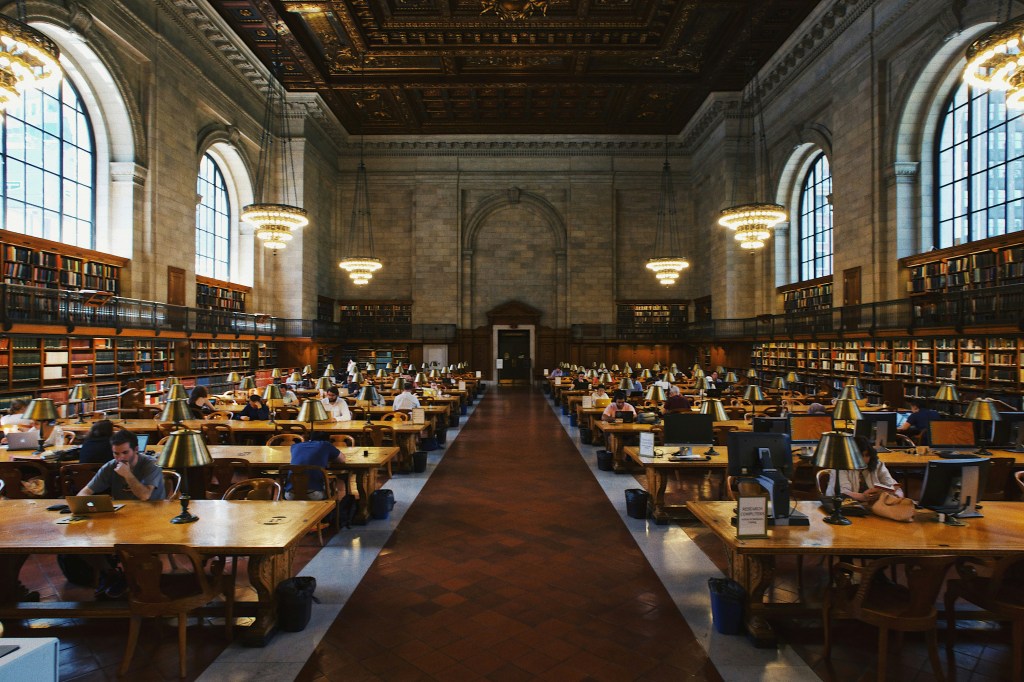
Why a Team Approach Matters
Managing diabetes in athletes requires teamwork.
The athlete, doctor, athletic trainer, coach, and family all play a role.
The athletic trainer helps prevent and handle blood sugar problems during sports.
Diabetes Care Plan
Every athlete with diabetes needs a care plan. This includes:
- How to check blood sugar
- Insulin guidelines
- Medication list
- Signs of low and high blood sugar
- Emergency contacts
- Wearing a medical alert tag
Essential Supplies for Athletes
Trainers should keep these in their kit:
- Blood sugar monitor
- Glucose tablets or juice for low blood sugar
- Glucagon for severe low blood sugar
- Ketone test strips
- Spare insulin pump parts
Health Checks Before Sports
Athletes with diabetes need regular check-ups:
- HbA1c every 3-4 months
- Yearly eye and kidney exams
- Heart health screenings
- Urine tests for ketones or infections

Managing Blood Sugar
Low Blood Sugar (<70 mg/dL)
- Causes: Too much insulin, exercise, or missed meals
- Prevention: Check blood sugar often, eat enough carbs, adjust insulin
- Treatment:
- Mild cases: 10-15g of fast-acting carbs (juice, glucose tabs)
- Severe cases: Glucagon injection, call for help
High Blood Sugar (>250 mg/dL)
- Causes: Not enough insulin, stress, illness
- Prevention: Take insulin as prescribed, check blood sugar often
- Treatment:
- Avoid exercise if ketones are present
- Stay hydrated
- Adjust insulin if needed
Using Insulin
Types of insulin:
- Rapid-acting: Works fast (lispro, aspart)
- Short-acting: Regular insulin
- Intermediate: NPH
- Long-acting: Lasts all day (glargine, detemir)
Ways to take insulin:
- Multiple daily injections (MDI)
- Insulin pump
Adjusting Insulin for Exercise
- Reduce basal insulin (pump) 1-2 hours before exercise
- Reduce mealtime insulin by up to 50%
- Pause pump during short workouts
Medication and Supplies
- Insulin: Main treatment
- Glucagon: For severe low blood sugar
- Carbs: Juice, glucose tablets for mild lows
- Ketone tests: Check for ketoacidosis
- Emergency kit: Extra insulin, blood sugar supplies

Exercise Tips
- Check blood sugar before, during, and after exercise
- Eat carbs based on activity level
- Watch for low blood sugar hours after activity
- Adjust insulin based on workout intensity
Traveling with Diabetes
- Keep supplies in carry-on luggage
- Bring extra insulin and prescriptions
- Wear a medical ID
- Plan for time zone changes and meal timing
- Learn emergency phrases in the local language
Injuries and Blood Sugar Control
- Injuries can raise blood sugar
- High blood sugar slows healing
- Check blood sugar often when injured
Weather and Diabetes
- Hot and cold weather affects insulin
- Check blood sugar more often in extreme conditions
- Don’t apply heat or cold to injection sites
Preventing Long-Term Complications
- Eye exams every year
- Kidney function tests every year
- Foot exams for nerve damage
- Heart screenings for older athletes or those with risk factors
Staying Safe
- Regular blood sugar checks
- Right insulin doses
- Proper diet
- Good communication with the care team
- Know the signs of high and low blood sugar
Emergency Planning
- Team members should know emergency steps
- Keep emergency supplies nearby
- Be ready to give glucagon if needed
- Have a plan to call emergency services

Long-Term Success
- Regular HbA1c tests
- Ongoing education and support
- Keep the care plan updated
- Monitor for long-term health problems
Managing diabetes in sports takes planning, but with the right approach, athletes can perform at their best.