Definition
- Definition
- Clinical Anatomy
- Characteristics
- Differentiation between Type A and Type B Lower Crossed Syndrome:
- Exam
- Management
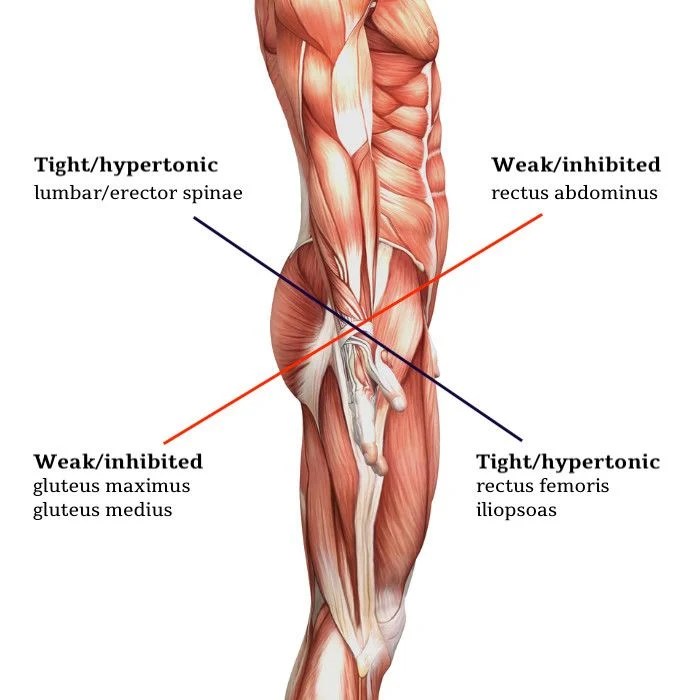
Lower crossed syndrome (LCS), also termed Unterkreuz, pelvic crossed, or distal crossed syndrome, presents as a neuromuscular imbalance characterized by overactive hip flexors and lumbar extensors coupled with weak abdominal and gluteal muscles.
This pattern typically results in anterior pelvic tilt, hip flexion, and lumbar hyperlordosis, often accompanied by tight hamstrings.
The condition reflects a systematic muscular imbalance crossing between the body’s dorsal and ventral aspects
Clinical Anatomy
The clinically relevant anatomy of lower crossed syndrome involves two key muscle groups:
Inhibited/Weak Muscles:
- Trunk muscles (rectus abdominis, internal/external obliques, transversus abdominis)
- Gluteal complex (maximus, medius, minimus)
Overactive/Tight Muscles:
- Thoracolumbar extensors (erector spinae, multifidus, quadratus lumborum, latissimus dorsi)
- Hip flexors (iliopsoas, tensor fasciae latae)
- Hamstrings (compensatory for anterior pelvic tilt/inhibited gluteus maximus)
This muscular imbalance creates a pattern of dysfunction where superficial muscles compensate for deeper muscular weakness.
Characteristics
Clinical presentation of lower crossed syndrome involves:
Key Joint Effects:
- Ligamentous strain at L4-L5, L5-S1 segments
- Increased pressure on SI and hip joints
- Pain in lower back, hip, and knee
Postural Changes:
- Primary: anterior pelvic tilt, increased lumbar lordosis, lateral lumbar shift, hip external rotation, knee hyperextension
- Secondary: increased thoracic kyphosis, increased cervical lordosis
Two Subtypes:
- Type A: Primarily affects hip
- Type B: Primarily affects lower back
Associated Features:
- Diaphragm and transversus abdominis imbalance
- Underactive deep transversus
- Variable activity in obliques and rectus muscles
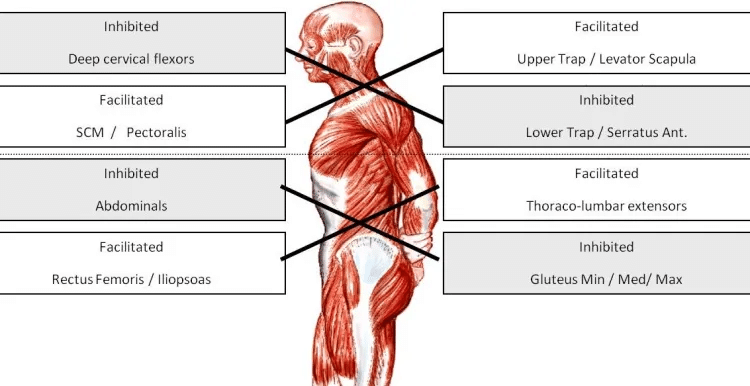
Differentiation between Type A and Type B Lower Crossed Syndrome:
Type A (Posterior Pelvic):
- Dominated by axial extensor
- Overactive back muscles lead to increased lumbar curve and anterior pelvic tilt
- Because the hip flexors are shortened, the pelvis is tilted anteriorly and the hip and knee are in slight flexion.
- Anterior pelvic tilt with hip/knee flexion
- Hyperlordosis of L spine and hyperkyphosis in the transition from T to L spine
- Anterior thorax translation and Increased thoracolumbar extension
- Breathing pattern: upper chest with shortened expiration
- Shortened expiration with poor diaphragm-abdominal coordination
- Primary issue: respiratory dysfunction: Compromised breathing patterns affect core stability and posture
- Poor intra-abdominal pressure
- Overactive psoas
- Infra-sternal angle >90°
- Limited costo-vertebral movement
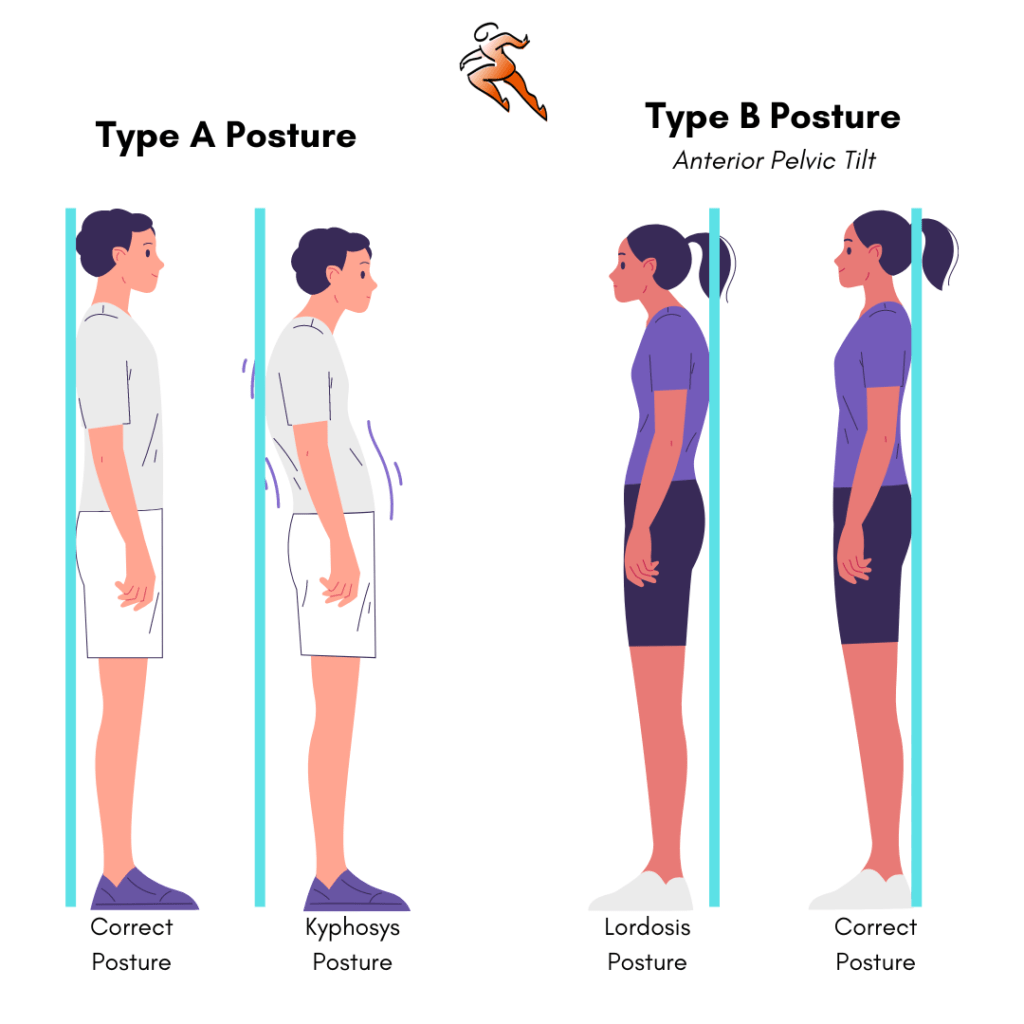
Type B (Anterior Pelvic):
- Dominated by axial flexor
- Trunk flexors overpower extensors, altering spinal alignment
- Weak/short abdominals
- Muscles are both functionally weak and adaptively shortened
- Minimal lumbar hypolordosis
- Thoracic hyperkyphosis
- Head protraction
- Forward head posture from thoracic curve compensation
- Anterior pelvis position
- Knee hyperextension
Exam
Standing Assessment:
- Check pelvic tilt (typically anterior)
- Observe lumbar lordosis
- Assess tightened/inhibited muscles tone patterns
Active Tests:
- Hip extension (straight leg lifting)
- Hip abduction (watch for rotation/flexion compensation)
- Trunk curl-up (iliopsoas/abdominal interaction)
Passive Tests:
- Hip flexors: Modified Thomas test
- Hamstrings: Straight leg raise
- Adductors: Supine at plinth edge
- Piriformis: Supine rotation test
- Quadratus lumborum: Side-lying trunk bend
- Spinal erectors: Short-sit forward bend
- Triceps surae: Ankle dorsiflexion (target 90°)
Key Assessment Points:
- Check soft tissue resistance
- Note range of motion limitations
- Observe compensatory patterns
- Document pain responses
Management
Treatment Principles:
- Focus on stretching tight muscles vs strengthening
- Stretching improves antagonist strength via reciprocal innervation
- Hold stretches 15 seconds
- 5-week active stretching improves ROM
Key Stretches:
- Iliopsoas
- Erector Spinae
Additional Interventions:
- Soft Tissue:
- Myofascial release and/or Trigger point therapy
- Laser/ultrasound for gluteus/TFL
- Core Training:
- Abdominal strengthening
- Lumbar mobility work
- Pelvic control exercises
Posterior Type Focus:
- Improve active exhalation
- Train caudal thorax movement
- Progress from supported to unsupported positions
- Maintain neutral spine
- Build intra-abdominal pressure with proper breathing